What is CRYOSURGERY?
Cryosurgery/Cryotherapy is the new treatment that offers unbeatable results in prostate cancer, without the need for complicated surgical procedures.
It is the 3rd generation of cryotherapy systems with all the latest innovations of the last 10 years, with a technique and machinery guaranteed by all the certificates of the FDA and CE.
It is a system of freezing and thawing of tissues susceptible to be destroyed by means of argon and helium, respectively. This treatment is very safe, due to the ability to control freezing, avoiding damaging unwanted areas.
Maintains a continuous and detailed control of the cold sensitive areas: external sphincter, bladder neck and anterior rectum through a system of monitored thermocouples, and is a surgical technique that allows a hospital stay of 24 hours and without bleeding.
Cryosurgery/Cryotherapy is one of the few techniques that can be repeated, either by PSA elevations or cancer persistence, but not in others such as radical prostatectomy or any form of radiotherapy.
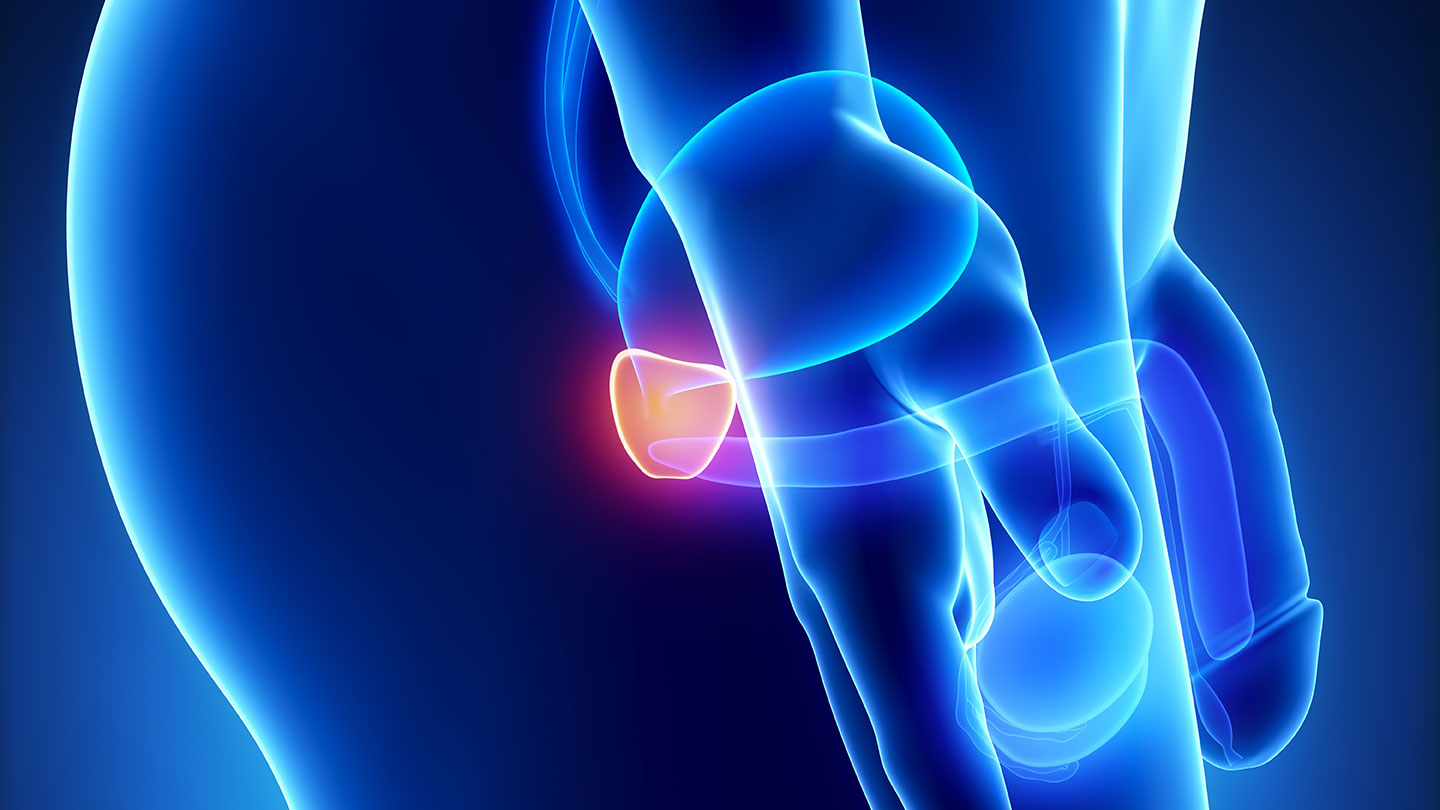
Prostatic cryosurgery
Cryosurgery, also called cryotherapy or cryoablation, is used to treat prostate cancer by freezing cancer cells with cryoprobes.
Advantages of cryosurgery
- Hospital admission minimum between 12 and 24 hours.
- No need for blood transfusions, and a FAST RECOVERY of normal activity.
- Lower morbidity, with incidence of urinary incontinence less than 1% (High quality of life index).
- Without the undesirable effects of radiation in the short and long term of Radiotherapy and Brachytherapy.
- Possibility of repeating the surgery if a cancer cell persists, without additional risk to the patient.
- It can be used as rescue therapy for failures of other techniques such as Radiotherapy-Brachytherapy.
Prostate cryosurgery
Prostate cryosurgery is the cellular process that involves controlled freezing of the prostate gland to destroy cancer cells. The damage caused by freezing occurs at several levels: molecular, cellular, and the complete tissue structure. Important factors that influence freezing are the rate of temperature reduction once the procedure is started, the time the cells remain frozen, and the rate of heating during thawing.
Cells are not the only structures that suffer damage during freezing. During the cryoablation of the prostate, the surrounding connective tissue (stroma) and small blood vessels (capillaries) are also damaged, so that after the procedure they suffer from an insufficient supply of blood that is believed to slow the growth of the cancer.
Cryosurgery Technique
Cryosurgery is a surgical procedure performed in the operating room with the anesthetized patient.
The technique involves inserting an ultrasound probe through the rectum to obtain an accurate image of the prostate.
Under continuous monitoring through the images of the sonography, a few crio ablation probes are placed whose mission is to freeze the prostate and destroy all the tumor cells due to the extreme cold obtained.
epidural or general anesthesia is required during this procedure.
Mechanism of action
The purpose of this complex process is to maintain total control of the area to be treated but without affecting the important organs adjacent to the prostate.
The most significant advantage of this new technique in relation to the previous ones used in the 90s, is the use of Argon gas for freezing and Helium gas for rapid heating (the temperature of the probe can go from -186ºc to 40ºc in 30 seconds).
During cryosurgery, two freezing cycles are usually applied.
Indications
Patients with high and medium risk of periprostatic infiltration with 2 or 3 of the following factors:
- PSA greater than or equal to 10, Gleason greater than or equal to 7, Stage T2b-T3a.
- Patients with cancer limited to the gland with low risk of extracapsular extension:
- Stage T1b-T2a, PSA <or equal to 10, Gleason <or equal to 6, multiple pathologies, high surgical risk.
- Alternative to surgery and radiation in patients with low risk of extracapsular cancer.
- Patients with coagulation disorders.
- Patients who do not consent to receive blood transfusions.
- Patients with resistant or recurrent cancer after brachytherapy and / or external radiotherapy.
- Patients with extracapsular cancer (T3).
- In patients with unilateral cancer, unifocal and low risk of extracapsular extension: to try to avoid impotence while preserving the neuro-vascular band on one side.